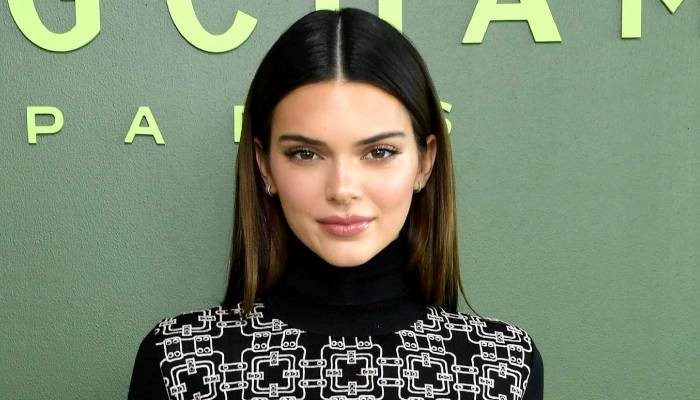
In patients with asthma and type 2 diabetes, certain newer classes of antidiabetic agents were associated with a higher incidence of acute exacerbations when compared with metformin, a retrospective population-based cohort study from Japan found. Both DPP-4 inhibitors and GLP-1 receptor agonists were linked with a higher incidence of exacerbations requiring systemic corticosteroids versus metformin, reported Yuya Kimura, MD, of the University of Tokyo, and colleagues: • DPP-4 inhibitors: 18.2 vs 17.4 per 100 person-years (HR 1.09, 95% CI 1.05-1.14) • GLP-1 agonists: 24.9 vs 19.0 per 100 person-years (HR 1.14, 95% CI 1.01-1.28) However, patients taking SGLT2 inhibitors had similar incidences of asthma exacerbations that required use of systemic corticosteroids compared with metformin (17.3 vs 18.1 per 100 person-years, respectively; HR 1.00, 95% CI 0.97-1.03), they wrote in the Journal of Allergy and Clinical Immunology: In Practiceopens in a new tab or window. As for exacerbations leading to hospitalization, only DPP-4 inhibitors were significantly associated with a higher incidence rate compared with metformin (0.52 vs 0.38 per 100 person-years; HR 1.44, 95% CI 1.15-1.81). Metformin has long been the first-line option for treating type 2 diabetes, noted Kimura and co-authors in their introduction, but American Diabetes Association guidelinesopens in a new tab or window now recommended GLP-1 agonists or SGLT2 inhibitors "as first-line drugs for patients with specific complications (atherosclerotic cardiovascular disease, heart failure, and chronic kidney disease)." "Metformin and these novel antihyperglycemic drugs are assumed to have direct anti-inflammatory effects, not only due to better glucose control, but also due to their intrinsic pharmacological actions," the researchers continued. "The anti-inflammatory effects of these drugs, alongside improvements in glycemic control and systemic changes in metabolism (i.e., weight reduction), may contribute to better control of chronic lower respiratory diseases, such as asthma and chronic obstructive pulmonary disease (COPD), where chronic respiratory inflammation is associated with poor disease control." The new findings contrast with prior research. One previous study in asthma patientsopens in a new tab or window showed that those initiating GLP-1 agonists for diabetes had lower numbers of exacerbations compared with those starting on SGLT2 inhibitors or DPP-4 inhibitors, though the analysis included a smaller number of patients on these newer drugs and did not evaluate metformin as a comparator. Rekha B. Kumar, MD, of Weill Cornell Medicine and NewYork-Presbyterian Hospital in New York City, told MedPage Today in an email that she expected SGLT2 inhibitors to be effective for controlling asthma, noting that providers who see opportunities for use in patients with asthma and conditions like diabetes or heart failure may now feel more comfortable using them. However, she said that the lack of asthma control associated with use of DPP-4 inhibitors and GLP-1 receptor agonists was somewhat surprising. "This shows us that the mechanism of asthma control is very complex and medicines that are novel for weight loss and blood sugar control don't always benefit all organs, such as the lungs," she noted. "We always thought the relationship between these drugs and asthma would be linked to weight, but that does not appear to be true based on this study." Kimura and colleagues used data from the National Database of Health Insurance Claims and Specific Health Checkups, which includes data from 99% of Japan's hospitals, to construct three active comparators, including new user cohorts of patients with a history of asthma starting the novel antidiabetic drugs and metformin from January 2014 through December 2022. For the DPP-4 inhibitor analysis, 46,024 new users of these drugs and 18,256 new users of metformin were included. Mean age was 58.9, and 46.5% were women. During the follow-up period of 97,475 patient-years, 18,740 first exacerbations requiring use of systemic corticosteroids occurred. For the GLP-1 agonist analysis, the authors included 1,948 new users of these drugs and 20,914 new users of metformin. Mean age was 56.2, and 55.4% were women. During the follow-up period of 33,978 patient-years, 5,749 first exacerbations requiring use of systemic corticosteroids occurred. For the SGLT2 inhibitor analysis, 35,397 patients who were starting these drugs and 35,648 patients starting metformin were included. Mean age was 59.6, and 44.7% were women. Over the follow-up of 99,485 patient-years, 17,767 first exacerbations requiring use of systemic corticosteroids occurred. In secondary analyses, there were no differences between subgroups for age, sex, body mass index, HbA1c level, triglyceride level, and low-density lipoprotein cholesterol level, among others. Kimura and colleagues acknowledged that the study's observational design was a limitation. They also noted that they only included patients from Japan, which could have limited the generalizability of their findings.